How do you know if you have Diastasis Recti and what can you do about it?
What IS Diastasis Recti?
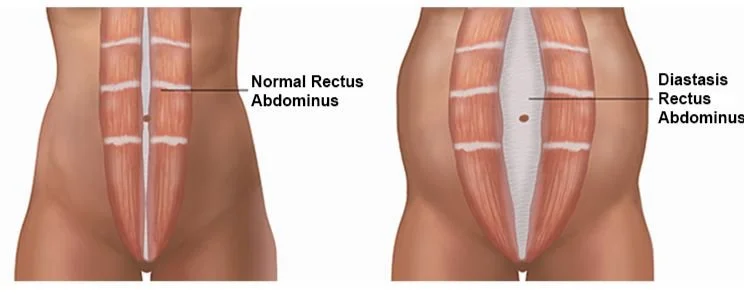
Did you know that diastasis recti is unavoidable during pregnancy? Every pregnant woman will experience some degree of diastasis recti by their third trimester. Diastasis recti aka abdominal separation is the stretching of your linea alba - or the connective tissue that runs down the middle of your most superficial core muscle, the rectus abdominis. The rectus abdominis is often referred to as the “six pack” muscle and is separated into two muscle bellies. The linea alba is what connects these muscle bellies. This tissue stretches because your baby is growing and your body needs to make room. Diastasis recti is a normal adaptation to pregnancy and is just one example of how amazing and resilient our bodies truly are.
Diastasis recti becomes problematic when it lingers into postpartum. For many women, diastasis recti will naturally heal with time. However, there are certain risk factors and lifestyle habits that can influence the ability for your diastasis recti to fully heal. Some risk factors include:
Cesarean sections
If you’ve had multiple pregnancies close together
If you are pregnant with multiples
Higher BMI
Core weakness/general deconditioning
High intensity exercise like HIIT, cross fit and heavy weight lifting too soon after having a baby or doing these activities during pregnancy without the deep core strength and pressure management strategies to support you (we will get into this)
So how do you know if you have it Postpartum?
Some will get checked by their birthing provider or PT. You can also do a self-exam at home:
Start by lying on your back with your knees bent, head rested flat on bed/floor
Place two fingers along the midline of your abdomen, about an inch or two above your belly button.
See if you can feel the edges of both muscle bellies - this may be less obvious for some, and you may need to dig around a little. *Remember, your rectus abdominis is separated into two muscle bellies with a line of connective tissue running vertically in between them - from your sternum to your pubic bone
While keeping fingers along the midline of your abdomen, in between your muscle bellies, lift your head and shoulders off the ground without flexing your stomach muscles.
Feel for any gap getting wider or deeper.
Repeat this about an inch or two below your belly button and at the level of your belly button. Diastasis recti can present at any and all three of these levels so it’s good to check them all.
You likely have some diastasis recti if:
Your can fit 3 or more fingers inside the gap
Your finger can sink down to your first knuckle or deeper
You see a doming or coning along the midline of your abdomen:
Abdominal Doming often looks like a small football is bulging out of the midline of your abdomen. For some it can be quite obvious, for others it can be more subtle.
You may also hear the term Abdominal Coning. Coning and Doming are essentially one in the same - coning tends to look like a more narrow protrusion just a long your midline.
And how do you get rid of it?
Typically, a combination of exercise and lifestyle changes. It’s often recommended that one include deep core strengthening to treat diastasis recti. While I don’t disagree with this sentiment and do recommend starting here, you want to make sure you eventually progress beyond just deep core work.
When most refer to the “deep core” we are referring to the Transverse Abdominis (TrA) muscle. This muscle helps generate tension along your abdominals and acts like a corset. Many of us are disconnected to this muscle, which is why I recommend first learning how to turn it on. However, once you have good control of your TrA, you want to start working OTHER core muscles including the more superficial muscles like your rectus abdominis.
It was once thought that if you used your rectus abdominis muscles to do things like crunches or planks, this would worsen your diastasis. However, we are finding that if you are able to recruit your TrA while doing these exercises (so you don’t have abdominal doming/coning), they are not only safe but a critical part of your recovery.
Why? Because the core muscles do not work in isolation. You can think of the core like a canister: you have the abdominal muscle layers comprising the front part of your can, your lower back muscles comprising the back part of your can, your oblique muscles comprising the sides of your can, your diaphragm comprising the top of your can and the pelvic floor supporting the bottom. If you don’t have good strength across all of these muscles, your core canister can become dysfunctional and lead to issues like pain, urinary leakage, prolapse, persistent diastasis recti, etc.
So how do you do deep core work and how do you know when you are ready to progress? It’s hard to discern on your own therefore I recommend working with a Pelvic Floor Physical Therapist so they can ensure you are effectively engaging your deep core and can help provide you with a customized exercise plan as you are ready for more challenge. Psst - this is something we can treat virtually so please book a consult if you are needing support!
And what should you avoid if you have Diastasis Recti?
There is a LOT of fear mongering and misconceptions around Diastasis Recti. And research is continually changing. This makes it hard for even us clinicians to stay on top of best practices. That being said, please make sure you are getting your advice from a licensed professional who has extensive training around postpartum conditions like Diastsis Recti.
You do want to avoid exercises or activities that reproduce the abdominal coning or doming. Sometimes you are able to resolve the coning/doming with engagement of your deep core muscles. If you are able to resolve it, then you can continue that activity but remain focused on your deep core.
You also want to avoid holding your breath while doing things like having a bowel movement, lifting your baby, exercising, etc. This is because if you are not managing your intra-abdominal pressures properly, activities that add pressure to your system can worsen your separation. Start to bring attention to how you are breathing during these activities and practice “exhaling on your exertion” aka the hard part of the movement.
Lastly, it’s helpful to manage constipation. Because constipation leads to straining which puts excessive force through your core canister. Like mentioned above, when having a bowel movement, make sure you avoid straining and perform an exhale as you gently bear down. Using a squatty potty or step stool works great too.
So I don’t need surgery?
I’m going to be honest - it really depends on the severity of your diastasis, what your symptoms are like and what your goals are. Typically, I’m only recommending surgery if you are unsatisfied with the look of your diastasis and you’ve already been working with a Pelvic Floor PT for at least 6 months. If your abdominal separation is severe, exercise alone will unlikely help with the appearance of your separation however it can help with function/symptoms. Surgery is not all that common but sometimes warranted! There’s no shame in getting a procedure done if this helps your confidence and improves your overall quality of life.
Summary of Treatment Options:
If you have confirmed or think you have Diastasis Recti, don’t be alarmed! You have options and you don’t have to do it alone. Your treatment plan should include deep core strengthening followed by a progression of core work including the major muscle groups that support your core canister: the transverse abdominis, rectus abdominis, obliques, multifidi, pelvic floor, glutes and diaphragm. You should also be working on pressure management strategies during exercise and day to day activities.
If you are pregnant or plan to get pregnant soon:
Sign up for our birth prep course: OPTimize Birth. You will learn many strategies to safely strengthen your core canister and reduce forces going through your abdominal wall during birth. You will also have access to our exercise library which includes core exercises for each trimester - all which will help prevent your likelihood of persistent diastasis recti postpartum
If you are postpartum:
Keep an eye out for our upcoming postpartum course and book a virtual visit with Dr. Amanda, our licensed Pelvic Health Physical Therapist.
Seek out a local Pelvic Floor Physical Therapist (if you are in the Portland-Metro area you can inquire about in-person appointments with Dr. Amanda)